Human Growth Hormone (HGH) Therapy for IBD
Introduction to Human Growth Hormone Human Growth Hormone (HGH) is mostly known for the dubious claim that it can slow aging, as well as its use by bodybuilders to accelerate muscle growth. HGH is an important hormone that stimulates and regulates our body’s growth and cell reproduction. Some people have HGH deficiencies, leading to stunted […]
Introduction to Human Growth Hormone
Human Growth Hormone (HGH) is mostly known for the dubious claim that it can slow aging, as well as its use by bodybuilders to accelerate muscle growth.
HGH is an important hormone that stimulates and regulates our body’s growth and cell reproduction. Some people have HGH deficiencies, leading to stunted growth. They supplement it to make up for the condition, increasing bone density and muscle mass. It is also used to treat complications from HIV/AIDS that lead to muscle degradation.
HGH is also a potential therapy for irritable bowel disease because of the connection between inflammation and HGH resistance, as well as the potential of HGH to heal damaged cells that are either damaged by or lead to IBD.
The degenerative effects of inflammatory bowel disease
The compromised gut barrier function in inflammatory bowel disease (IBD) is associated with decreased nutrient uptake and malnutrition.1 Combined with increased energy consumption by the disease-related activities, it leads to over-activation of catabolic pathways.2 These pathways break down large macromolecules of our body, such as proteins, into smaller molecules, and generate energy.
Corticosteroids, which are used to suppress inflammation as a treatment for IBD, have catabolic effects (where the body is breaking tissue down, versus an anabolic state, where it’s building up tissue) on body composition that include bone demineralisation, growth delay, fat mass increase and insulin resistance.34
As a result of these catabolic effects, about 40% of pediatric patients with Crohn’s disease (CD) show growth impairments, often leading to short stature in adulthood.5
IBD drains structural resources of the body, which manifests itself in loss of proteins and deterioration of muscles and bones. These effects can be counteracted and treated by inducing anabolic pathways.6 This is an outline of the framework and current literature related to the usage of HGH or Growth Hormone for treating IBD.
What is HGH?
Human Growth Hormone (HGH) is a small protein molecule that is made naturally by our pituitary gland and secreted into the bloodstream. As its name suggests, it was originally known to regulate childhood growth.7 Nowadays, its physiological effects are acknowledged to be broader than that. Those effects can be direct or indirect.89
Direct and indirect effects of HGH
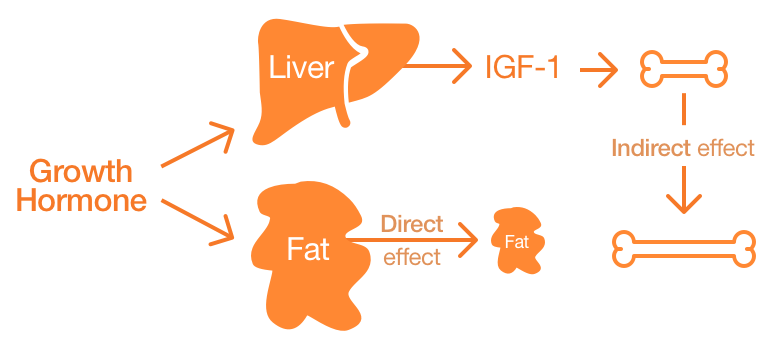
The breakdown of large molecules, such as fats, provide energy needed for many bodily activities.
Direct effects occur due to the binding of HGH to its cognate receptor on cells and inducing changes at cellular and tissue physiology. For example, adipocytes (fat cells) have receptors for HGH. When HGH binds to these receptors, adipocytes break down triglyceride (a prominent fat molecule) and they are blocked from swallowing and accumulating circulating lipids.10 This activity may account for the observed shrinkage of fat mass in HGH-treated patients.
Indirect effects are those that are not caused by the HGH itself, but by other molecules that become available when HGH levels are high (Figure 1). For example, IGF-1 (Insulin-like growth factor-1), which is secreted by hepatocytes11 when HGH levels are increased in the body, is a molecule that induces these indirect effects of HGH.12 Such IGF-1 related indirect effects could be inhibiting apoptosis (cell death) of existing cells, thereby increasing their lifespan.13
HGH also has significant metabolic functions, mainly via IGF-1. HGH causes cells to enter an anabolic state14 with respect to protein metabolism. In this way, our body obtains large molecules needed for new cells, as well as storing unused energy. Newer cells are required for tissue and organ growth and regeneration. Since IBD damages intestinal tissues, their regeneration is critical, and this process could be facilitated with anabolic reactions.15
A synthetic, or recombinant, form of HGH called somatropin was developed in 1985 and is very similar to the natural form.1617 This synthetic version can also stimulate tissue growth, linear growth (height), as well as protein, carbohydrate, lipid, and mineral metabolism.18
How does HGH work for IBD?
As noted earlier, HGH is a natural molecule that can induce anabolic processes in our cells, growing and regenerating tissues, while catabolic pathways lead to the breakdown of larger molecules into smaller molecules to generate energy. As it can lead to the shrinking of tissues and organs, the balance between anabolic and catabolic reactions is critical.
IBD patients, especially those on corticosteroid therapy, have increased catabolic activity, like excessive protein breakdown and protein loss. HGH can, the theory goes, reverse these effects for patients with IBD.
HGH potentially can have a direct effect on cells within the bowel and induce desirable responses for IBD like:19
- Mucosal integrity, renewal, repair by acting on epithelial cells.20
- Wound healing by acting on mesenchymal cells.21
- Modulating inflammation by acting on intestinal immune cells.
According to DePascalis et al., HGH and IGF-I together are considered to be key determinants to “promote wound healing and growth of the intestine by increasing cell proliferation and collagen deposition.” Chronic inflammation in IBD damages intestinal tissues and results in their disintegration. Since collagen is the key structural protein in our extracellular matrix (ECM) and required for the survival of cells, collagen deposition contributes to rebuilding the intestinal tissue.
The FDA has approved HGH for treatment of adult short bowel syndrome, which is “…a disorder that affects people who have had large portions of their small intestine surgically removed as a result of a digestive illness, such as Crohn’s disease…” because of its beneficial anabolic effects.22 HGH treatment could also be helpful for children with IBD to prevent growth delays caused by factors like malnutrition.
Is HGH legal?
Human Growth Hormone is an active ingredient in several drugs approved by the FDA for treatment of a limited number of diseases. The FDA says that “HGH products are new drugs and cannot be legally marketed in the U.S. without an approved application.” The FDA does not approve the active ingredients themselves, only the drugs that include them. Therefore, it is illegal to use HGH for treating conditions other than those it can be prescribed for:
- Hormonal deficiency that causes short stature in children
- Long-term treatment of growth failure due to lack of exogenous growth hormone secretion
- Long-term treatment of short stature associated with Turner syndrome
- Adult short bowel syndrome
- Adult deficiency due to rare pituitary tumors or their treatment
- Muscle-wasting disease associated with HIV/AIDS
HGH is not approved currently by the FDA for the direct treatment of IBD.
Studies on HGH therapy for IBD
The record of clinical studies that use HGH as a treatment for Crohn’s and colitis goes back more than 40 years. In a small-scale 1974 study at the University of Chicago Clinical Research Center by McCaffery et al., researchers applied HGH to three IBD patients.23 The researchers based their investigation on a previous study that observed low HGH levels in severely growth-retarded children with inflammatory bowel disease.
Patients received 10mg of HGH daily for the first five days, after which the dosage was reduced to 3mg and three times a week for the next six months. Although two of the patients saw their height increase by 4.5cm and 4.7cm, respectively, the authors concluded that this was not a true growth advancement that could be expected from growth hormone therapy. The patients’ growth rate had not exceeded their predicted growth rate. The third patient showed negligible growth while on the HGH treatment.
Researchers also examined the effects of HGH treatment on nitrogen balance in these patients. Positive nitrogen balance during the course of the treatment indicated that patients were showing an anabolic response to the HGH treatment. We shouldn’t consider the catabolic effects of steroid drugs in these patients because two of the patients had never received steroids, while the other one had quit six months before the study began. In the absence of the catabolic effects of steroids, the anabolic effect that HGH generates may not be enough to produce notable changes in stature. In any case, the number of patients involved in this study was too low for results to be completely reliable.24
Studies on HGH for Crohn’s disease
In a clinical study published in the New England Journal of Medicine, one of the most respected journals in clinical research, researchers applied HGH to adult patients25 with moderate-to-severe active Crohn’s disease.26 The study was carried out at North Shore University Hospital and New York University School of Medicine, both in New York.
One of the salient features of this study is that the 37 assigned patients were divided randomly into two groups; one receiving the real treatment (i.e., the HGH) and the other a placebo (a similar solution, not including HGH). The aforementioned study lacked such a placebo control, which is vital for researchers to discern the effect of an active substance from other confounding factors.
Another important factor is that the patients were following a high-protein diet. IBD patients suffer from protein breakdown and protein loss, likely due to malnutrition. The high-protein diet could balance the protein levels in the body and complement them with HGH to induce the anabolic processes required for the restoration/regeneration of the intestinal barrier’s integrity.
Patients self-administered subcutaneous injections of HGH – 5mg per day for the first week and 1.5mg per day after that – or a placebo for four months. At the end of the four months, patients were evaluated according to the Crohn’s Disease Activity Index. The HGH-injected group showed a significant reduction in their score when compared to the placebo group, which indicated a decrease in the severity of the disease.
Among the eight variables investigated by researchers in the scope of the Crohn’s Disease Activity Index, they found a significant improvement on three of the variables in the HGH group, but none in the placebo group:
- The number of liquid or very soft stools per day
- Severity of abdominal pain
- Overall well-being
The five other variables were not different from baseline values. The authors concluded that HGH might be a beneficial treatment for patients with Crohn’s disease, but were unable to confirm that conclusively.27
Studies with children
According to a report in the European Journal of Pediatrics in 1996, three adolescent patients (aged 14-17) with Crohn’s disease were treated with recombinant growth hormone (HGH) for two years at the University of Technology Dresden’s Department of Paediatrics.28 As a result, all three patients showed increased growth velocity and advanced bone age. But the authors concluded that part of the therapeutic benefit may have been caused by the onset of puberty in the patients.
In another clinical study, performed at the Wolfson Children’s Hospital in Jacksonville, Florida, ten children – six boys and four girls – were treated subcutaneously with 0.05mg/kg of recombinant HGH per day for at least six months.29 Nine of the children had Crohn’s disease and one had a form of nonspecific IBD compatible with autoimmune enteritis – a rare autoimmune disorder that causes intestinal inflammation and long-lasting diarrhea in children. Children received oral prednisone (a steroid). The authors concluded that “the administration of rhGH (HGH) to glucocorticosteroid-treated growing children has beneficial effects on whole body metabolism and linear growth while the child remains on steroids.”
Supporting this conclusion, children had a higher fat-free mass and a lower percentage of fat mass as a result of the treatment, indicating the metabolic benefits of HGH treatment. Additionally, linear growth velocity – that is, they got taller – reached 7.7cm/yr after six months of combined prednisone and HGH treatment, up from 3.5cm/yr when the patients were being treated with only prednisone. The authors emphasize that HGH “should not be considered a treatment for the disease itself but rather for some of its chronic complications, mostly related to steroid use.”30
In a pilot study conducted between August 1990 and March 1994 at the New England Medical Center (now Tufts Medical Center) in Boston, seven children – six boys and one girl31 with Crohn’s disease and growth failure were enrolled.32
In the first year, four patients received a placebo, and the other three received HGH (0.05mg/kg per day). In the second year, all patients received HGH. Overall, the authors observed no significant improvement in growth or nutritional status. However, two of the patients who received HGH therapy in combination with nutritional support grew taller. One of the patients was given Elemental 028 and clear liquids (in total, 2400kcal/d) and the other patient received nocturnal nasogastric tube feedings of three boxes of Nutrin – peanut extract – a day (in total, 1500kcal) in addition to HGH.
The results suggest that HGH treatment needs adequate nutritional support to show benefits. Again, the sample size in this study were too small to reach final conclusions.33
According to a report published in the Journal of Pediatrics, ten children and adolescents34 with Crohn’s disease and deficient growth were treated subcutaneously with open label35 recombinant growth hormone at 0.043mg/kg/day for one year at the Pediatric Clinical Research Center at UCSF.36 Although this study was not controlled with a placebo group, the authors used retrospective data of patients matched for age and sex as a comparison group.
As a result, researchers observed that the HGH-treated group had a significantly higher growth rate (5.33cm/yr) during their year taking HGH versus the comparison group (0.96cm/yr). HGH treatment also increased bone mineralization, which is an important problem in children with chronic disease, indicating that HGH can have anabolic benefits.
Despite these benefits, patients didn’t show any clinical improvement in disease activity.37
Researchers from Cincinnati Children’s Hospital Medical Center (CCHMC) enrolled twenty patients aged 7-18 with active Crohn’s disease who were already receiving corticosteroids (CTX) in a randomized controlled clinical trial of HGH.38 The first group received 0.075mg/kg/day of HGH alongside CTX for 12 weeks, while the second group39 received CTX alone. The dosage of the HGH used in this study was notably higher than the average of other studies.
After 12 weeks, researchers examined clinical and endoscopic disease activity, while the control group also began receiving HGH. Their clinical disease activities were evaluated at 24 weeks. For those who were showing clinical response, researchers extended the therapy an extra 52 weeks, after which their height was assessed.
Results showed that the HGH-receiving group had a higher linear growth and improved clinical disease activity (reduced symptoms) when compared to the control group.
Researchers examined whether HGH treatment confers any benefit in the regeneration of the mucosal tissue to counteract the disintegration caused by IBD. But neither healing nor reduction of inflammation were observed in either group.
The authors concluded that HGH “was safe and effective as an adjunct to CTX for treatment of clinical disease activity and growth failure in pediatric CD [Crohn’s disease].” However, there were two weaknesses in this study: the majority of the patients were male, making it harder to generalize the findings to include females, and second, the control group did not receive a placebo injection, so the placebo effect could have confounded the results.40
Studies on HGH for ulcerative colitis
I have only encountered one study about HGH treatment with ulcerative colitis patients.
It was was carried out in Denmark with 24 patients41 undergoing ileoanal J-pouch surgery.4243 It was double-blind, randomized, and placebo-controlled study, which greatly increases the reliability of the data.
The balance between anabolic and catabolic processes is critical. As we’ve observed, anabolic processes favor the synthesis of complex molecules and the growth of tissues and organs, while, catabolic processes favor the degradation of complex molecules into simpler ones, while generating energy. For example, increased catabolic response is associated with surgical morbidity rate.44 Additionally, protein loss, muscle wasting and muscle weakness are some catabolic effects which are associated with surgical stress.45 In this study, researchers hypothesized that metabolic effects of HGH would counteract the aforementioned consequences of the disease and the surgical operation.
Patients were given either 12 lU/day46 HGH or placebo treatment from two days before to seven days after surgery. The patients receiving HGH showed less reduction in muscle strength at postoperative days 10, 30, and 90 and less fatigue at days 30 and 90, while regained more lean tissue mass at day 90.
Although this study was performed under special circumstances – on surgical patients – its results indicate that HGH could be helpful in inducing anabolic effects on ulcerative colitis patients.47
Is HGH safe?
In the the safety findings I collected from different clinical studies, HGH treatment was found to be mostly safe without any substantial adverse effects, but there are two limitations to safety of any study that you should bear in mind.
One of them is the HGH dose taken by the patients during the study. Any adverse event or lack of an observed one is only valid based on the dosage used in the study. Higher dosages than used in the study may yield other side effects. We can’t know one way or the other.
Another is the sample size, or the number of patients included in the study. As the sample size increases, it becomes more representative of the whole population and the collected data is more reliable.
As you will see below in the summary of the safety findings I collected from different clinical studies, mostly, HGH treatment was safe without any important adverse effects.
HGH side effects
Slonim et al. performed an HGH study in 37 adult patients48 with Crohn’s disease. This was a placebo-controlled study, as patients were divided randomly between HGH and placebo treated groups. All these provide evidence for us to rely on the results.
The low dose of HGH used in this study should be noted (0.5mg/kg/week for the first week, 0.15mg/kg/week for the rest of the 16 weeks).49 There were no serious side effects that necessitated the patient’s withdrawal from the study. Edema50 and headaches were the most frequent side effects, and they disappeared in the first month. One patient developed arthralgia (joint pain). Another patient showed enlarged, tender lymph nodes, possibly due to a reduction in the dosage of growth hormone, and breast tenderness.
Researchers discovered tumors in three patients, but concluded that they were not related to the HGH therapy as one was detected in a patient within the placebo group and the two in the HGH group were detected at the initial phase of the therapy.51
The UCSF study published in 2008 observed no adverse effect of HGH in any of the patients,5253 but the small sample size of ten patients and low injection dose (0.043mg/kg/day) could have affected results.
In a recent study at the Cincinnati Children’s Hospital Medical Center (CCHMC), authors concluded that HGH “was well tolerated with no unexpected safety signals… in the setting of moderately active pediatric Crohn’s disease.”54
Mild injection site discomfort was the most frequently observed adverse event. Some other adverse events observed were an increase in fasting insulin55 at the extension phase (treatment was extended for those who showed clinical response at initial phase), intracranial hypertension56, peripheral edema57 and arthralgias (joint pain).
Twenty patients, ages 7-18, were included in this study and the HGH dose was higher than in other studies (at 0.075mg/kg/day).58
In a seven-patient (ages 11-16) study employing 0.05mg/kg daily dose of HGH, Calenda et al. observed “itching at the injection site and mild erythema59 in one of the patients at the initiation of GH therapy which resolved after a change in the vehicle6061 No side effects were observed in other patients.
Hannon et al., which studied eight adolescent62 Crohn’s disease patients, concluded that none of the reported adverse events, such as flare-ups of Crohn’s disease and one new case of asthma, were caused by the HGH treatment (0.35mg/kg/week).63
Ten patients (average age, 11.9 years) were injected with 0.05mg/kg/day HGH for six months at Wolfson Children’s Hospital at Jacksonville, Florida.64 HGH was tolerated well as no adverse events were reported. Only one patient “had an acute enteritis during the first month secondary to Clostridium difficile (C-dif) bacteria, which responded to antibiotic treatment.”
Although no significant adverse effects were associated with the usage of HGH in IBD patients, not all studies of HGH were neutral in this regard. Takala et al. reported a placebo-controlled study on hundreds of patients who had been in intensive care unit for several days due to a multitude of reasons, such as cardiac surgery, abdominal surgery, multiple trauma, or acute respiratory failure. The results indicated that the mortality rate was higher in patients who received growth hormone than those who were treated with placebo.65
According to Ken Ho, an endocrinologist from Australia, patients who take HGH for unapproved purposes “develop diabetes, heart failure and severe disfigurement of the face, from the development of huge ears, a large nose and protruding jaw and their quality of life is totally miserable.”
HGH gut
Have you ever wondered why so many muscular men in bodybuilding circles look pregnant? This condition is characterized by extreme swelling of the belly, which many in bodybuilding circles speculate to be caused by excessive HGH or insulin use. They call it bubble gut, GH gut, roid belly, and other interesting names.
Bodybuilders use HGH with the aim of increasing muscle mass, despite the fact that scientists do not agree with this claim.66 Similarly, there is no scientific evidence that links abdominal bloating to HGH. Some say that it may be caused by increased growth of abdominal muscles as a result of HGH treatment.
But scientific studies point out that, while HGH can stimulate the growth of connective tissue, it does not induce muscle growth in otherwise healthy people.67
We could assume that the dosage used by the athletes might be higher than that used in the scientific studies, which may explain the difference, but we can neither assess whether they consistently do so nor if that would affect the outcome.
Methods of HGH delivery
HGH can be taken in a number of ways, not all of them are effective or recommended. Injections were the standard method of delivery in the aforementioned studies.
HGH injections
HGH injections can be done in two ways: intramuscularly (IM) and subcutaneously (under the skin) – in prescribed uses.
In the clinical studies targeting IBD patients, subcutaneous injection was the preferred method of HGH delivery. Injections can also be done by the patients themselves.68
HGH gel
Although HGH is available in gel form as skincare product, its effects (both intended and side effects) have not been evaluated by the FDA. Regardless, it is intended to prevent wrinkles and indications of aging on the skin. No clear usage exists for IBD treatment.
HGH supplements
Certain studies indicate that supplements, such as melatonin, glutamine, ornithine, creatine, L-dopa and glycine can boost HGH production naturally.
However, the duration of the effect seems to be short-lived.
They are typically taken for three to six months, followed by a rest period of the same length, where it is claimed that HGH levels remain steady.
HGH pills
HGH pills are supplements taken in pill form to, supposedly, increase HGH production. See above.
SeroVital hGH
SeroVital hGH is not an actual HGH product. It is a blend of specific amino acids that is claimed to boost HGH production.
Currently, we’re not sure whether uptaking those amino acids could improve IBD symptoms.
The HGH cycle
There are many websites claiming that HGH should be received in a “cycle,” a specified duration of HGH intake followed by a period of no intake, for certain benefits like anti-aging or muscle building. They recommend different cycle length and dosage for different health goals.
Please be aware that these are not legally approved usages and no approved cycle or dosage exists for IBD at the moment.
Conclusion
There are just under ten clinical studies which evaluated the benefits and side effects of HGH as an IBD treatment. Most of them used pediatric patients as a subject. In some, there were no control groups. However, there are studies observing adult patients that were designed adequately so as to be scientifically reliable.
Overall, these studies support the hypothesis that HGH has anabolic effects. Stature growth (in pediatric patients), positive nitrogen balance, increased bone mineralization, muscle mass, fat free lean mass, and decreased fat mass are the findings that indicate the anabolic response to HGH treatment.
In two controlled studies, significant improvement was observed in clinical disease activity. However, no study suggested healing of the inflamed tissue or a reduction in inflammation, which are the main causes of IBD symptoms.
In addition, two other studies suggested that HGH treatment could be more effective with nutritional support, especially via a high-protein diet.69
HGH should not be considered as a stand-alone treatment for IBD. The data suggests that it may have benefits as a supportive agent, especially with an aim to reduce the negative consequences of the steroid drugs. Further clinical research is necessary to assess the benefits of HGH for IBD patients.
- Capristo E., Eur. Rev. Med. Pharmacol. Sci., 3(4), 111-113 (1998).
- Capristo E., Eur. Rev. Med. Pharmacol. Sci., 3(4), 111-113 (1998).
- Mauras N., Metabolism, 51 (1), 127-135 (2002).
- Capristo E., Eur. Rev. Med. Pharmacol. Sci., 3(4), 111-113 (1998).
- Heyman M.B., J Pediatr., 153 (5), 651-658 (2008).
- Which build complex molecules from simpler ones, such as proteins from amino acids.
- Brinkman J.E., Sharma S., StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 (2018).
- Brinkman J.E., Sharma S., StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 (2018).
- Growth Hormone (Somatotropin). (n.d.). Retrieved November 26, 2018, from http://www.vivo.colostate.edu/hbooks/pathphys/endocrine/hypopit/gh.html
- See above.
- Main cells of the liver which perform crucial metabolic functions
- See above
- Brinkman J.E., Sharma S., StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 (2018).
- Recall that anabolic reactions are the part of the metabolism that builds complex molecules from simpler ones, like proteins from amino acids.
- Brinkman J.E., Sharma S., StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 (2018).
- See WebMD for more
- And the FDA listing
- See FDA, above.
- De Pascalis B. et al., Eur. Rev. Med. Pharmacol. Sci., 10, 13-16 (2006)
- The innermost layer of the cells in the gut that are exposed first-hand to the gut lumen and digestive processes that occur there.
- These include different types of cells, such as fibroblasts and myofibroblasts, which originate in the mesoderm in embryo. They reside in the intestinal tissues, as wells as other tissues of the adult human, and play critical roles in physiological processes such as inflammation and wound healing.
- De Pascalis B. et al., Eur. Rev. Med. Pharmacol. Sci., 10, 13-16 (2006).
- McCaffery T.D. et al., Digestive Diseases, 19(5), 411-416 (1974).
- McCaffery T.D. et al., Digestive Diseases, 19(5), 411-416 (1974).
- Mean age, about 40 years.
- Slonim A.E. et al., N Engl J Med., 342 (22), 1633-7 (2000).
- Slonim A.E. et al., N Engl J Med., 342 (22), 1633-7 (2000).
- Henker J., Eur J Pediatr., 155 (12), 1066-7 (1996).
- Mauras N., Metabolism, 51 (1), 127-135 (2002).
- Mauras N., Metabolism, 51 (1), 127-135 (2002).
- Ages, 11.9–16y
- Calenda K.A., Inflamm. Bowel Dis., 11 (5), 435-441 (2005).
- Calenda K.A., Inflamm. Bowel Dis., 11 (5), 435-441 (2005).
- 12.6±4.5 years; six male
- In an open label type of clinical study, both researchers and patients are aware what treatment was given. Therefore, results cannot be claimed to be purely unbiased.
- Heyman M.B., J Pediatr., 153 (5), 651-658 (2008).
- Heyman M.B., J Pediatr., 153 (5), 651-658 (2008).
- Denson L.A. et. al., J Pediatr Gastroenterol Nutr., 51 (2), 130-139 (2010).
- The control group.
- Denson L.A. et. al., J Pediatr Gastroenterol Nutr., 51 (2), 130-139 (2010).
- Mean age, 31 for HGH and 35 for placebo.
- A type of surgery employed generally for ulcerative colitis patients that involve the removal of colon and rectum and attaching the end of the small intestine (ileum) to the anus
- Kissmeyer-Nielsen P. et al. Ann. Surg., 229 (2), 298-302 (1999).
- Kissmeyer-Nielsen P. et al. Ann. Surg., 229 (2), 298-302 (1999).
- Kissmeyer-Nielsen P. et al. Ann. Surg., 229 (2), 298-302 (1999).
- International Units
- Kissmeyer-Nielsen P. et al. Ann. Surg., 229 (2), 298-302 (1999).
- Average age, ~40 years
- Slonim A.E. et al., N Engl J Med., 342 (22), 1633-7 (2000).
- Swelling that can occur in different parts of the body. It is caused by excess fluid accumulated in underlying tissues
- Slonim A.E. et al., N Engl J Med., 342 (22), 1633-7 (2000).
- Average age, 12.6
- Heyman M.B., J Pediatr., 153 (5), 651-658 (2008).
- Denson L.A. et. al., J Pediatr Gastroenterol Nutr., 51 (2), 130-139 (2010).
- A high level of fasting insulin indicates the insulin resistance – insulin doesn’t show its effects – and may cause high levels of glucose.
- High pressure within the spaces that surround the brain and the spinal cord. Complications may include permanent vision loss.
- Swelling mainly in lower legs, feets and ankles, as well as in arms and hands
- Denson L.A. et. al., J Pediatr Gastroenterol Nutr., 51 (2), 130-139 (2010).
- Redness of the skin caused by increased blood flow.
- A solution, a pill or any other formulation used to carry drug into action site.
- Calenda K.A., Inflamm. Bowel Dis., 11 (5), 435-441 (2005).
- Ages 13.7–21.2
- Hannon, T.S., J. Pediatr. Endocr. Met., 24 (9-10), 633-40 (2011).
- Mauras N., Metabolism, 51 (1), 127-135 (2002).
- Takala J., The NEJM, 341 (11), 785-92 (1999).
- Rennie M., Br J Sports Med., 37(2), 100-105 (2003).
- Doessing S., J. Physiol., 88(Pt 2), 341–351 (2010).
- Slonim A.E. et al., N Engl J Med., 342 (22), 1633-7 (2000).
- Though not specifically endorsed by any of these studies, we wrote about a specific high-protein diet, Carnivore. -Ed

Comments