The Carnivore Diet for Inflammatory Bowel Disease (IBD)
The Carnivore Diet is a member of the low-carb, high-fat (LCHF) diet family. Although not universally adopted by the science or medical community, and with a potentially complicated transition, it has had nearly universally positive results for those with Crohn’s, UC, and IBS dedicated enough to try it.
Paleolithic and Ketogenic Diets: The Roots of Carnivore
Modern society has always been obsessed with fad workouts and diets. The ketogenic and paleolithic diets have recently become two of the trendiest, and many who suffer with IBS or IBD have found some solace with them. Recently many dieters and professionals have put them together to obtain the advantages of both. What research and experience has found, however, is that combining the two can provide even more benefits, particularly to those with Crohn’s and ulcerative colitis. This diet focuses on animals and animal byproducts and is formally called the paleolithic ketogenic diet, when adhered to strictly it’s also called the zero carb diet, or, more colorfully, The Carnivore Diet.
The Evolution of Our Guts: Where Did The Carnivore Diet Come From?
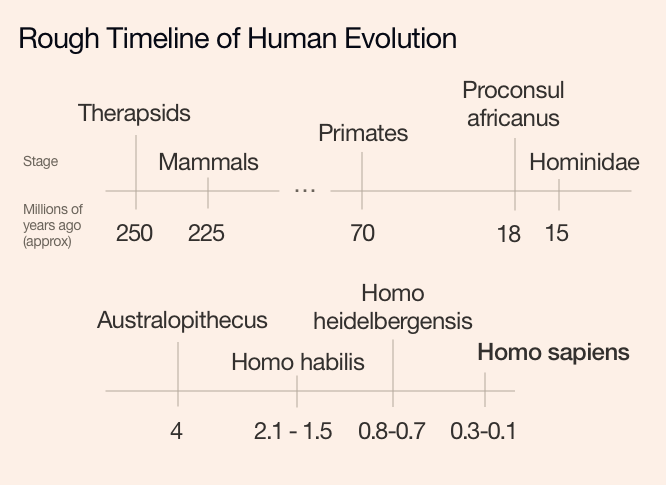
About 250 million years before we became concerned in removing gluten, carbs, meat, animal byproducts, pork, shellfish, fat, lactose, processed foods, peanuts, anything that our ancestors ostensibly didn’t eat, and fried food from our diets, the Earth went through the Permian–Triassic extinction event, which began the dying off of our ancestors at the time, the carnivorous therapsids.
The first mammals appeared a little later, 225 million years BP (before present). And we, Australopithecus at the time, separated from the chimpanzee somewhere between twelve and five, but probably around six or seven, million years before the invention of the deep fryer.
What we consider human first showed up with Homo habilis between 2.1 and 1.5 million years BP. H. habilis is the first to be associated with proper carved stone tools, although they had been around in some form for a million years or so, give or take a few 100,000. Homo habilis begat Homo erectus, who famously created fire and later cooking. They in turn begat Homo heidelbergensis, who may have invented clothing. Homo sapiens – that’s us – first showed up about 100 to 300,000 years BP and learned to speak.
It’s hard to say when talking about evolution where exactly to mark when we had the best diet or the most influential moment of evolution for our modern guts. We’re unsure exactly when our ancestors ate meat, but we do know that chimpanzees, our closest living relatives which are 94-99% genetically identical to us, are eager hunters, in contrast to earlier observations (a group of chimpanzees can consume up to a ton of meat annually given the chance).1 How much meat we ate in the course of our evolution, how we acquired it, and how frequently we ate it are all interesting questions open to conjecture and debate among scientists.
Our gut microbes have been shown to shift rapidly after certain events, such as the invention of tools, major shifts in our eating patterns, like settled agriculture, or a change in climate, and our guts have proven to be remarkably flexible and adaptable to what was available or practical at the time. In the modern day, we just eat whatever is trendy like jello salads2 or fondue3 If you have IBS or an IBD, you should probably stay away from glitter coffee anyway.
As the Paleo diet points out, all of these trends, including wheat, are recent. Until 10,000 BP, around the time we started farming, we had been in an ice age for 2.6 million years. Access to plants dropped drastically while research has shown that animal density was quite high. The amount of meat in our diet skyrocketed while the earth was engulfed in cold and we began to use tools to hunt. It is very possible, maybe probable, that our guts adjusted to being more carnivore than omnivore or herbivore from eating mostly meat in the cold for nearly all of the most recent two-point-six million years.
The Most Efficient Cure for Everything: The Effects of The Carnivore Diet
About 25,000 years ago the ancestors of the Native Americans, or First Nations if your flag’s a maple, crossed the Bering strait on a land bridge called Beringia. While braving the coldest part of an already freezing planet they were forced to develop a diet of utility that still remained 25,000 years later when the Europeans arrived.4 They were largely carnivorous and famously stressed the consumption of the entire animal. It was a diet high in fat and organs5, and is most directly represented in modern day by the Inuit, who have some summer vegetation but rarely touch it, save the occasional bit for seasoning. Although they do sometimes consume large amounts of berries, in a seasonal way similar to how we sometimes consume large amounts of pumpkin spice.
Dr. Joseph Romig was an important figure in Alaska at the turn of the last century and known as the “Dog-Team Doctor” because of his frequent house calls by dog sled and “Yung-Cha-wista” (Re-maker of People) by the Yup’ik. He reported that, other than the influenza, in the 36 years he had administered to the Yup’ik, he had “never seen a case of malignant disease among the truly primitive Eskimos … although it frequently occurs when they become modernized.”
Weston A. Price, dentist extraordinaire, performed quite a bit of fieldwork in the 1920’s and 30’s for his book “Nutrition and Physical Degeneration,” during which he interviewed Romig and wrote the quote above. His most interesting observations were, likewise, about the Native American diet.6 He claimed that he had even witnessed Native Americans contract influenza and survive by returning to their homes to follow their traditional lifestyle and consume traditional foods.
There have been more recent studies, several in the last ten years. A 1972 study on Point Hope, Alaska found that average total caloric content was 3,000 kcal per person. 50% of those calories were fat, 30-35% were from protein, and 15-20% were carbohydrates, but those carbs were mostly from glycogen (animal starch) in meat. Glucose was largely limited to tea or coffee sweetener, something that did not exist in their traditional diet.
The results of this research found that heart disease among residents of Point Hope was ten times lower than the US average. The levels of fat in their bloodstream were measured as 85 mg/dl, down from an average of 100 mg/dl. This was from a diet that consumed 50% fat. They were found to rapidly gain weight and cholesterol while moving towards a more western diet.
There has also been recent research on the Masai of East Africa, where only one male had a heart attack out of the 600 that were studied. They had a diet of 66% pure animal fat, that’s 300 grams of fat and 600mg of cholesterol every day. For reference, Americans are advised to keep cholesterol under 300mg, 20-35% of calories.
Other total or near-total meat-eating cultures include the Eurasian Steppe Nomads, the Gauchos of Brazil, Russian Arctic Chukchi, and the Sioux of South Dakota.
Hungarian clinical researchers Zsófia Clemens and Csaba Tóth of Paleomedicina are two of the world’s most prominent experts on Homo sapiens who are carnivorous. Paleo was adopted very quickly in their country as a treatment for a large number of people for whom an inadequate healthcare system did not have capacity. Because they were such early adopters, and in such large quantities, Hungarian physicians quickly accrued a large quantity of observations and data on the effects of the paleo diet that allowed them to make adjustments and learn from observation of individuals, many of whom were children, that experienced different physiological reactions. Their adjustments and research inevitably led them to the carnivore diet, which they refer to on their website as “the most effective tool for the treatment of the diseases of civilization.”
Paleomedicina has been researching Carnivore since long before it was cool.
The Science and Research of Carnivore for General Use, IBD, and IBS
Over 20 years ago, Robert Atkins put forward the Atkins diet, in the family of diet known as low-carb, high-fat (LCHF) (LCHF). Doctors and scientists were naturally skeptical of something that was generally described by their community as something that will kill you.
Even though many medical professionals practiced it themselves, they were wary to prescribe. The research wasn’t there and the perceived risk was too great. At that time, we really knew very little about the diet or how our bodies digested and absorbed what they needed. Today, physicians readily prescribe a low carb diet to their patients as a temporary diet or a lifestyle change, having observed or experienced the sustained effects themselves. Many IBD sufferers have gone on and off of it with success, not only with pronounced weight loss, but relief from IBS.
Here’s the thing. Despite a mountain of success stories, research, and acceptance from the medical community, in the nearly 50 years (since 1972) of its existence, what we call the Atkins diet has never been fully confirmed by science, particularly in the long-term. For weight loss, The Lancet questioned its central claim, that burning fat offers a metabolic advantage over burning carbohydrates, concluding that the weight loss was a result of a reduction in caloric intake due to to the monotony of the diet.7 Weight loss, however, is incidental to our aims.
As for mortality, if a patient on Atkins dies tomorrow or at 90 we will never know if their diet was the cause.
Another LCHF diet, specific carbohydrate diet (SCD) has been in use since the 1950’s and because of that, has extensively more evidence on its results for those with Crohn’s and UC.
The carnivore diet is a combination of the ketogenic and paleolithic diets and shares a lot of their characteristics and benefits, but works in many different ways. It also shares similarities and overlaps with the specific carbohydrate diet (SCD) and low FODMAP (Fermentable Oligo-, Di-, Mono-saccharides and Polyols) diet which have been well researched for their relief of IBS and IBD. Eating meat alone actually overlaps with quite a few diets, but those are the most relevant and familiar to those of us with IBS and IBD.
FODMAP works by limiting high FODMAP foods that would otherwise be difficult for some of us to digest until they are fermented by the gut bacteria at the end of the intestines that produce hydrogen and lead to gas, bloating, cramps, general pain, constipation, and many psychological issues such as anxiety and depression. It’s useful because it can isolate and discover particular foods that may be causing problems. As with many gut issues, different foods are offenders for different people. The removal of all potentially FODMAP producing foods is the most restrictive, but then they can be reintegrated slowly so that each individual can discover their own personal demons.
Carnivore is a much more serious reduction, and it’s suggested you start by removing everything but meat. Then slowly add things like dairy, coffee, and perhaps alcohol. In some schools of carnivore thought you can even experiment with adding limited vegetables.
Carnivore has the most in common with keto, and shares a similar goal of reaching ketosis in order to switch from a carb-based metabolism to a fat-based metabolism. There has also been research that the state of ketosis causes enhanced mental clarity and focus8. It shares with paleo the prevention and cure for problems caused by carbohydrates and additives. When the two are combined as carnivore, there are even more interesting changes to our bodies, as well as our IBS and IBD.
Paleomedicina suggests that, while the paleolithic diet removes excessive carbohydrates and additives and the ketogenic diet puts the body into ketosis, neither address the very thing that truly makes the paleolithic ketogenic diet unique and why it has massive application if you have an IBD or IBS: intestinal permeability.
Our intestines are meant to be permeable. Intercellular tight junctions are supposed to allow nutrients to be absorbed while keeping antigens out. Today, those junctions are generally open too wide, enough that disease is able to stay within our body rather than being forced out as intended.
Increased intestinal permeability leads to more disease and more harmful diseases, and those are a big problem, but of more concern to IBS, UC and pancolitis. The body responds to the invaders by triggering the immune system and increasing inflammation. As we keep seeing on Guthack, it’s generally agreed that IBD could be caused by a genetic predisposition to unusual immune responses while reacting to certain bacteria.
To quote from our excellent article about FMT:
“There is a current consensus among literature that IBD is very likely caused by a genetic predisposition to an unusual immune response to certain bacteria (endoluminal). These bacteria have been shown to alter the development of anti-inflammatory T-regulatory cells and pro-inflammatory cells.”
Guthack: Fecal Microbiota Transplant (FMT) for Inflammatory Bowel Disease (IBD)
That alteration leads to inflammation. For those visitors who might not be familiar with IBD, the I stands for inflammatory.
Although the link is not clear, increased intestinal permeability is also known to be a cause of Crohn’s, UC, IBS, and pancolitis. For the rest of you, increased intestinal permeability is also linked to diabetes, arthritis, fatty liver, joint diseases, obesity, liver problems, allergies, schizophrenia, and even cancer.
The Paleomedicina Clinic offers extensive resources on the subject, but beware, the site is only partially in English and does not always play well with Google translate.
Nutrition is often a personal discovery, while there is an abundance of work about how nutrition should affect humanity as a whole, ultimately, each of our bodies work differently of our genetics, environment, lifestyle, upbringing, health history, and a biochemistry that identifies us all as uniquely as a fingerprint. Those of us who suffer from diseases such as IBS, Crohn’s, ulcerative colitis, or pancolitis have our own factors that make us different. In an absence of greater research, we can feel better trying it on our own to see how it applies to our own personal biology. Luckily, Sean Baker, one of the most notorious proponents of going carnivore, is working on just that and we hope to do the same for IBD and IBS, or anyone who wants to share their experience.
Whether or Not The Carnivore Diet is for You and Your IBD or IBS
If you’re on prescription drugs, have a doctor monitor your situation. Particularly with blood pressure, your body will be going through changes and that may make your prescription put you at dangerous levels.
If you have some sort of problem that precludes it, you have trouble adhering to things strictly, or staunchly object to consumption of animals and animal products, a perfectly valid objection, this diet is not for you.
Conclusion on The Carnivore Diet for Use with IBD, IBS and Everything Else
We find many diets seem to be complete opposites in appearance, but ultimately what is important is to match essential nutrients, not foods. If we know what we are eating and how that affects our bodies we don’t have to look for diversity in the food we consume. We only have to meet the body’s requirements.
Another great thing about eating carnivore is that you don’t have to worry if you don’t want to micromanage. There is no fake broccoli, mushroom, or soy product made entirely of meat. When you invest yourself in being carnivorous, you only eat one thing: meat. You can learn new techniques, cuts, sources, and seasonings as you go along, essentially picking up a new hobby.
Even if it isn’t for you, the Carnivore diet is safe to try and many Crohn’s and UC patients are experiencing full remission of problems that were considered permanent conditions. One of the most famous testimonies on the internet, Crohn’s Carnivore, reported that after six years of the diet, and three years since his last colonoscopy, his doctor found him to be indistinguishable from someone without Crohn’s.
The Carnivore diet is one of the most promising, safe, and surprisingly simple methods to relieve Crohn’s, Ulcerative Colitis, and Pancolitis. Eat meat. Eat when hungry. Eat until pain-free.
- The Predatory Behavior and Ecology of Wild Chimpanzees
- Popular in the 60s, “Gelatin salad is the Nehru jacket of the Thanksgiving menu: Outdated, and unlikely to come back into fashion.”
- Also popular in the 60s. We were all born in the 80s. These examples can’t be explained. -Ed
- There’s a fantastic visualization of these early human migration patterns at the Bradshaw Foundation. Requires Flash and doesn’t work on mobile, so here’s a link to a video version.
- There is a fascinating and much debated piece on the topic, Guts and Grease: The Diet of Native Americans.
- Detailed writeup previoulsy linked above.
- “A systematic review of low-carbohydrate diets found that the weight loss achieved is associated with the duration of the diet and restriction of energy intake, but not with restriction of carbohydrates.”
- LaManna, J. C., Salem, N., Puchowicz, M., Erokwu, B., Koppaka, S., Flask, C., & Lee, Z. (2009). KETONES SUPPRESS BRAIN GLUCOSE CONSUMPTION. Advances in Experimental Medicine and Biology, 645, 301–306. http://doi.org/10.1007/978-0-387-85998-9_45
Comments
6 responses to “The Carnivore Diet for Inflammatory Bowel Disease (IBD)”
JN
The first sentence “The Carnivore Diet is a member of the Low Fat High Carb (LFHC) diet family…” should be LOW CARB, HIGH FAT (LCHF), no?
Interesting article otherwise. I’ve been almost completely free from IBS, chronic muscle pain/fibromyalgia, arthritis pain for almost 2 years and have lost over 90lbs by following a ketogenic diet, but I’m looking into carnivore as a next step in gut healing. Thanks for the info!
Yury Tsukerman
Thanks for the comment and great catch. It should be “low-carb, high-fat (LCHF)” – correct in the article itself. If you do start the diet, we’d love to hear how it goes vs. keto.
Patrick
I’m a 50 y/o fit male with UC since 2015. I’ve tried every diet out there with no reluef in symptoms until I went 100% carnivore. I”ve been carnivore for 6 months, and never felt better since diagnosed. However, my fecal calprotectin tests results continue to be high (>200) despite feeling better with hardly any symptoms. They are higher than when flaring at my worst. Any thoughts on why this is happening?
Yury Tsukerman
Really glad to hear that this diet has helped, but that is indeed a strange result (as they often are – it’s not a perfect solution). Have you spoken with your doctor?
Brit
I know this was 2 years ago, but I’d like to know if your doctor had any insight and if your fecal cal tests are lower now? I was diagnosed in 2017 with UC and have only had one flare, but have never really felt well. So many food restrictions and I’ve been thinking about trying keto or carnivore.
Jack Martin
I did SCD for several months, which resolved most of my issues(95%), but never a full resolution. However, I would still like to share my experience, in case it gives someone more confidence in dietary management. My fecal calprotectin was 3000 and CRP over 70, and I had excruciating pain and diarrhea (like 10 times a day). While waiting for a doctor, I tried SCD for myself, the first day, pain gone, literally, in about a year, my Calprotetin dropped to 76, CRP to 1.1, still inflamed, but 95% better. Oddly, my other markers especially liver related were all better. I was symptom free (my poop was just gorgeous then, once/day) until I started adding more food, and since then I have been having periodical minor pain in my gut, and stool would be a little loose during such times. Biomarkers are still fine, really mysterious, which is why I plan to try carnivore, just to see if it helps.
Low FODMAP Chocolate Peanut Butter Shake
If you’re a chocolate lover, then this is the ideal recipe for you!
Low FODMAP Chia Pudding with Raspberries
This Chia Pudding is one of the easiest and most versatile low FODMAP recipes you can make.
Alcohol and its Effects on IBD and IBS
If you’re suffering from irritable bowel syndrome or an inflammatory bowel disease, you might wonder if drinking alcohol is going to make your symptoms worse. You’ve probably heard that alcohol is bad for your gut, but not sure to what extent. Depending on your specific condition, we have reviewed the effects of alcohol revealed by recent scientific research.
The Best Probiotics for IBD and IBS: Everything You Need to Know!
Are probiotics effective for ulcerative colitis and Crohn’s? We’ll talk about about the role of bacteria in gut health, gut dysbiosis, the role of probiotics, and the best probiotics for IBS and IBD.
The Complete Guide to Ulcerative Colitis
Ulcerative colitis (UC) is one of two types of inflammatory bowel disease (IBD). UC, as its name implies, means ‘ulcers’ from inflammation of the colon or large intestine. UC can extend from the rectum up to the small intestine and can cause destruction of other organs.
Human Growth Hormone (HGH) Therapy for IBD
Introduction to Human Growth Hormone Human Growth Hormone (HGH) is mostly known for the dubious claim that it can slow aging, as well as its use by bodybuilders to accelerate muscle growth. HGH is an important hormone that stimulates and regulates our body’s growth and cell reproduction. Some people have HGH deficiencies, leading to stunted […]
Supplements for IBS and IBD: Is There Any Evidence?
Let’s delve into the details of what science says regarding the use of supplements for IBS and IBD to separate fact from myth.
Small Intestinal Bacterial Overgrowth (SIBO)
SIBO is a condition that brings about excess bacterial growth in the small bowel. Though there are many studies that have highlighted the efficacy of various treatments, more research needs to be done on other factors and alternative treatments that can prevent SIBO.
Symptoms of Crohn’s Disease in Females
Symptoms of Crohn’s disease in women are similar to men except that women are more prone to gynecologic disturbances in severe cases and may experience pregnancy difficulties if the symptoms are severe and the condition uncontrolled. Prompt diagnosis and treatment are essential for women throughout their reproductive years.
An Overview of Irritable Bowel Syndrome (IBS)
IBS affects 10-20% of the population and is considered a functional gastrointestinal (GI) disorder with symptoms of abdominal pain and excessive or infrequent bowel habits.
Irritable Bowel Syndrome (IBS) Symptoms in Women Aggravated by Hormones
Women have unique challenges to manage their IBS successfully. Symptoms of IBS in women vary wildly and underlying hormonal disturbances play a key role. There are multiple triggers that increase a woman’s susceptibility to flares of IBS.
The Specific Carbohydrate Diet (SCD Diet) for IBS and IBD
The Specific Carbohydrate Diet, or SCD Diet, is one of the longest researched lifestyle changes to alleviate life-threatening digestive issues. Beginning with the “Banana Diet,” developed nearly 100 years ago for children with celiac disease, the SCD diet quickly showed results for IBS and IBD.
Interview With Kristina Campbell, MSc, On The Gut Biome
An interview with gut biome expert, science writer Kristina Campbell (M.Sc.), the author of The Well-Fed Microbiome Cookbook and co-author of an academic textbook, Gut Microbiota: Interactive Effects on Nutrition and Health. She writes, consults, and works with scientific advisory boards for microbiome-related organizations throughout Europe and North America.
Questions and Criticisms about The Carnivore Diet for IBS and IBD
Answers to common questions about the Carnivore Diet, for everyone, not just for those with IBS and IBD.
The Low FODMAP Diet for IBS and IBD
The low FODMAP diet was originally researched to treat Crohn’s disease, but has since been shown to be even more effective in treating IBS. It is something that everyone who has IBS or IBD should try.
Cannabis to Treat Ulcerative Colitis and Crohn’s Disease
As many of us have realized, traditional treatments of ulcerative colitis, pancolitis, and Crohn’s disease are not effective for many patients. If you are not responding to traditional treatment or feel the medications you’re taking are doing more harm than good, you may want to consider using cannabis to treat your ulcerative colitis, pancolitis, or Crohn’s disease. Science has not yet demonstrated that cannabis is a cure. However, anecdotal evidence, the sheer number of patients with IBDs using marijuana, coupled with its low risk (besides legal in jurisdictions where it’s prohibited) and cost suggest that it’s worth trying if you haven’t responded to other treatments.
All about Gluten-Free Alcohol
If you’re suffering from irritable bowel syndrome or disease, you might wonder if there’s some miraculous way to get away with drinking alcohol. You likely already know to avoid alcohol as it may provoke an attack, but want to find a loophole. Depending on the specific condition, there may be certain types of alcohol that are safe, or at least safer.
How to Start and Stay on The Carnivore Diet for your IBD or IBS
An introduction, instructions, tips, plus a sample set menu to get on and stay on the Carnivore Diet. You’ll find it both easy: only eat meat and salt – and difficult: only eat meat and salt. We’ll walk you through it.
Fecal Microbiota Transplant (FMT) for Inflammatory Bowel Disease (IBD)
Fecal Microbiota Transplant (FMT) is a completely natural and safe process that, while a little weird, has led to remission of Crohn’s, Ulcerative Colitis, and IBS for many people. This is an introductory summary of what to expect, what you will need, and whether it’s for you.
Hyperbaric Oxygen Treatment (HBOT) for Inflammatory Bowel Disease (IBD)
Hyperbaric Oxygen Treatment is a technique famously used to heal decompression sickness or “the bends.” In the last decade it emerged as a safe treatment with success treating Crohn’s, Ulcerative Colitis, and IBS for many individuals.
Stem Cell Therapy as a Treatment for Inflammatory Bowel Disease
An introduction to stem cell therapy (SCT), a promising new treatment which offers new possibilities for relief from gastrointestinal disorders including ulcerative colitis, Crohn’s disease and IBS.