Supplements for IBS and IBD: Is There Any Evidence?
Let’s delve into the details of what science says regarding the use of supplements for IBS and IBD to separate fact from myth.
Being a gastroenterologist, I am bombarded with questions from my patients like, are supplements an option for my IBD? And is there science behind these supplements?
Let’s delve into the details of what science says regarding the use of supplements for IBS and IBD to separate fact from myth.
Top 4 supplement categories for IBS and IBD you should know about
While IBS and IBD are different conditions, they share quite a few similarities. The underlying problems that make you susceptible to these conditions can overlap. Understanding the trigger is the most important step towards managing your condition.
Below are the top four supplement categories for IBS and IBD.
The amazing gut microbiota, dysbiosis, and potent probiotics
Your gut is home to trillions of bacteria with the balance generally in favor of healthy or probiotic bacteria. These bacteria have remarkable health benefits, like keeping the mucosa of your gut healthy and the growth of bad bacteria under control.
One similarity between IBS and IBD is gut dysbiosis. Dysbiosis is a state in which the bad gut bacteria start to outgrow the good gut bacteria. The most commonly identified condition is the overgrowth of pathogens like E.coli, Streptococci, and Staphylococci in the gut.12345
This overgrowth, known as SIBO, leads to a multitude of side effects, which include increased local inflammation, enhanced levels of pro-inflammatory chemicals in the blood, aberrant intestinal permeability to toxins, increased oxidative stress, and so on. As a result, you can experience symptoms including bloating, indigestion, diarrhea or constipation, and flatulence.6
Probiotics
Probiotics are live bacteria that you can either take as a supplement or get from fermented foods. The idea of taking probiotics is to trigger the growth of gut-friendly bacteria. While there is a lot of pseudoscience surrounding probiotics and gut health, studies strongly support their use. The actual benefits depend on a number of variables. These include the probiotic strains used, the number of Colony Forming Units (CFUs), and the duration of treatment.
Here is a quick summary of randomized control trials (RCTs) and meta-analyses using probiotic supplements for IBS and IBD.
| Probiotic | Dose | Methodology | Results | References |
|---|---|---|---|---|
| VSL#312 | 900 Billion Units | The dataset included 119 Crohn’s sufferers, who within 30 days of ileocecal resection, were either given VSL#3 or similar placebo. Endoscopy was performed on day 90 and 365 to identify recurrence. | Although the two groups did not differ much at day 90, at day 365 the VSL group had significantly reduced recurrence and mucosal inflammation compared to the placebo. | Fedorak et al. 201511 |
| VSL#3 | Up to 1,800 Billion Units | A total of 29 patients were included that were randomized to receive either a combination of Ulcerative Colitis (UC) remission induction therapy plus VSL#3 vs. UC remission induction therapy plus similar placebo for 1 year. | In the VSL group, 93% of participants achieved successful remission after 1 year compared to only 36.4% in the placebo. group who achieved remission. | Miele et al. 2009 810 |
| Escherichia coli Nissle 1917 | 2.5–25×109 CFU | The study included 327 participants who were either given probiotics or mesalazine for 1 year. The success of remission maintenance and rate of relapse was measured among the participants. | The probiotic was superior even to the gold standard therapy in maintaining remission in UC patients with only 34% patients experiencing relapse compared to the 37% participants in the mesalazine group who had a relapse in a year. | Kruis et al. 20049 |
| Lactobacillus, Bifidobacterium, sp, etc.8 | 10-100 billion CFU | Meta-analysis identifying RCTs showing the efficacy of probiotics for symptom control in IBS. | Following are the main findings: -Ten trials showed a significant reduction in abdominal pain. -Eight trials showed a substantial reduction in bloating. -Six trials showed a reduction of flatulence. -Most of the trials showed improvement in diarrhea or constipation. | Moayyedi, et al. 20107 |
The following can be inferred from the data presented above:
- Probiotics are an excellent adjuvant (something that can you can take in addition to the usual therapy for added benefits) that you should consider adding to your routine in addition to your usual medical therapy.
- It generally takes longer for probiotics to take action than people think. Perhaps that’s the reason why many get frustrated when they don’t see results within a few days or even weeks. From personal experience and from recent research, it takes months or years for the probiotic therapy to reach full effect.
- The CFU number is quite important. The higher the CFU number, the more live bacteria reach the target areas. A good number would be more than 10 billion CFU.
- Combination probiotics are better than probiotics using single strains of bacteria.
Exacerbations and relapse of symptoms are rather common in IBS and IBD and often shows poor response to therapy. I have personally seen people finding symptomatic relief with regular probiotic treatment.
How does inflammation and immune activation come into play with supplements for IBS and IBD?
Another consistent feature of both IBS and IBD is chronic gut inflammation. In these conditions, there are a number of problems with the immune system that lead to a hyperactive inflammatory response. Let’s try to break that down.
How the immune system normally works
Any foreign object (an antigen) goes to a group of cells called the dendritic cells. The dendritic cells then interact with the naïve or undifferentiated T cells (immune cells). Based on the antigens, the T cells are either differentiated into Natural Killer Cell (NK-cells) or Th lymphocytes. The Th lymphocytes then increase the production of inflammatory chemicals like interleukins (IL), Tumor Necrotic Factor (TNF), interferons, nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) and so on.789
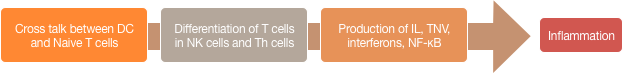
in NK cells and Th cells → Production of IL, TNV,
interferons, NF-κB → Inflammation
Inflammation is the key pathological event in IBD. Significant features include over-activation of the dendritic cells, accelerated differentiation of naïve cells into specialized inflammatory chemicals producing cells, and ultimately increased production of inflammatory chemicals such as IL, TNF, and interferons.101112
On that note, let’s talk about anti-inflammatory supplement options and the relevant clinical trials.
Is there enough evidence to support the use of curcumin (turmeric extract)?
Turmeric is a golden-yellow spice, native to South and Southeast Asia. Curcumin is the major bioactive component of turmeric and is responsible for giving it a bright, distinctive yellow color.

The basic anti-inflammatory action of curcumin in the perspective of IBD and IBS is its ability to stop NF-κB related immune activation and a subsequent reduction in the levels of inflammatory chemicals such as TNF, IL1, and IL2.13
Recall from the discussion above that inflammation is the major pathology in IBD and an anti-inflammatory agent like turmeric can be of value.
Turmeric for ulcerative colitis
In one meta-analysis conducted at the University of Minnesota, researchers studied the effects of curcumin-based therapies for management of IBD. The meta-analysis identified one major randomized controlled trial (RCT), which included 89 participants with ulcerative colitis who were randomized into two groups. In addition to the usual therapy with sulfasalazine and mesalamine, the participants either received 2g curcumin per day or a placebo.
At six months, only 4% of participants in the curcumin group experienced a relapse of symptoms compared to 16% of participants in the placebo group. At 12 months, the rate of relapse was still higher in the placebo group (32%) compared to the curcumin group (22%).14
Another RCT produced promising results when curcumin was used for remission induction in individuals with mild-to-moderate ulcerative colitis. The study included 50 patients with ulcerative colitis who either received 3g of curcumin per day in addition to their usual medical therapy, or a placebo. At four weeks, 54% of the curcumin group achieved remission, while none of the participants in the placebo group achieved remission.15
Table of on the efficacy of turmeric on IBS and IBD
Here are the details of RCTs evaluating the use of curcumin to manage IBS and IBD symptoms:
| Study Design | Results |
|---|---|
| This RCT included 500 participants with IBS who were randomly selected to take either 1 or 2 tablets of turmeric extract for 8 weeks.23 | The pain scores in both groups reduced by 20-25%. The quality of life (QoL) score improved between 5% and 36%. |
| This RCT was based on 99 participants who were randomized into two groups to either take placebo or IQP‐CL‐101 (a proprietary blend containing 330mg of curcuminoids)22. | The IBS Symptoms Severity Score (SS Score) reduced from the baseline of 315 to 202 at the end of 8 weeks in the IQP-CL-101 group. This is in comparison to 253 points at 8 weeks from 292 points at the baseline in the placebo group. |
The verdict on curcumin (turmeric)
So, what’s the final verdict? To take curcumin for IBS and IBD or not to take it?, The data available is quite promising, but large-scale studies are still needed to be sure whether curcumin (turmeric) has definitive benefits for IBS and IBD.
Are fish oil supplements as promising for IBS and IBD as claimed?
Fish oil is one of the richest sources of polyunsaturated fatty acids (PUFAs)- like omega-3 fatty acids. Essentially, there are three hypotheses as to how the use of fish oil might help with IBS and IBD.
First, the results of observational studies have shown that individuals with IBS and IBD are deficient in polyunsaturated fatty acids and their diets are generally inadequate in PUFAs as well. Second, PUFAs (as the ones coming from fish oil) have potent anti-inflammatory effects. They can block the production of interleukins and cytokines. Third, PUFAs help uphold the integrity of the intestinal mucosal barrier, reducing the spilling of toxins into the bloodstream that leads to aberrant immune and inflammatory responses.16, 17
In theory, the use of fish oil (or supplements containing PUFAs) can have significant benefits for people suffering from IBS and IBD. But actual evidence is somewhat scarce.
There are two large meta-analyses that have analyzed the efficacy of fish oil supplements in people with IBD. In one, researchers noticed only a small improvement in the symptoms of Crohn’s with the use of fish oil supplements but no similar benefit was noted in the UC sufferers.18
In another meta-analysis, researchers evaluated the effects of fish oil supplements in individuals with IBD in general. A total of 19 RCTs were studied and their results were analyzed. Unfortunately, none of the RCTs produced statistically significant results supporting the use of fish oil supplements for IBD remission induction, remission maintenance or control of symptoms.19
As for IBS, to the best of my knowledge and research, there are no major RCTs or meta-analyses that could prove any benefits of fish oil for IBS. However, there are a large number of observational studies and subjective accounts where PUFAs-based supplements have shown some benefit in relieving IBS symptoms like constipation or diarrhea, abdominal pain, and bloating.20
Verdict on fish oil
Final verdict? There is inadequate clinical and research evidence to support the use of fish oil supplements in IBS or IBD.
Does CBD Oil Help With IBS and IBD Symptoms?
Your body contains a system called the Endocannabinoid System (ECS). The ECS helps improve gut health and reduce inflammatory responses in the gut. This system includes the Cannabinoid Receptors: CB1 and CB2. These receptors are extensively expressed on the stomach, gut, and inflammatory cells.21 Researchers have noticed that mice deficient in CB1 and CB2 receptors have a higher risk of developing inflammation of the intestine.22
The evidence to support the use of cannabis for IBS and IBD is sparse. There has been only one RCT to support the use of cannabis-based products for IBD. In this study, 21 participants with active Crohn’s disease were randomly given cannabis containing cigarettes or placebos for eight weeks. At the end of eight weeks, 5 of 11 subjects in the cannabis group achieved complete remission, compared to only 1 out of 11 subjects in the placebo group.23
Verdict on CBD oil
The evidence to support the use of cannabis-based products or CBD oil for IBS and IBD is scarce. I see a lot of people in clinical practice saying that CBD oil and other marijuana-based products help immensely with their IBS or IBD symptoms. But the clinical evidence is still not convincing.
For a more in-depth look,
Do digestive enzymes help relieve IBS or IBD symptoms?
While malabsorption and maldigestion are not the major pathological features in IBD, these elements do play an important role in IBS. Researchers have noticed that individuals with IBD are more likely to suffer from idiopathic autoimmune pancreatic dysfunction compared to healthy individuals.24
If you have an IBD, you are more likely to be deficient in digestive enzymes. In IBS, the pancreatic amylases are deficient and this is becoming more recognized among IBS sufferers.25
Studies on digestive enzymes
There has been only one RCT that explores the beneficial role of digestive enzymes in IBD. This study was conducted at the University of Catanzaro, Italy and the participants included 43 IBD sufferers who also had IBS symptoms. Participants were randomized into two groups. In addition to the conventional therapy, one group (Group A) received a mix of beta-glucan, inositol, and digestive enzymes, containing lactase and cellulases, proteases and peptidases, nucleases, lipases, and carbohydrase amyloglucosidase. The other group (Group B) received a placebo in addition to the usual therapy for four consecutive weeks.
At the end of four weeks, Group A reported a significant decrease in symptoms, including bloating and flatulence. Most importantly, all patients in Group A reported a significant improvement in quality of life.26
Although the results are encouraging, there are some problems with the study design. Group A was given a combination of supplemental therapies, so we can’t say for sure if it was solely the digestive enzyme supplements that made the difference. The study was comprised of a small group and did not include a long-term follow-up. Finally, the relief provided by the digestive enzymes in IBS and IBD seems to be symptomatic. These supplements do a little to help relieve the underlying pathology.
Beano for IBS
One supplement that is worth specifically mentioning here is Beano, which helps your body break down complex carbohydrates.
How does Beano work?
People often wonder how exactly Beano works and whether it works for IBS. Well, the data available is scarce. Beano contains alpha-galactosidase (α-GAL), which is an enzyme that prevents the breakdown of sugars that would otherwise cause bloating, flatus, and abdominal pain.
Clinical trials involving Beano
There has been only one RCT that tested Beano. There have been no clinical trials to show the direct benefits of its use in IBS or IBD. This trial was done in 1994 at the University of California and included 19 participants, divided into two groups. Group One received drops of Beano and Group Two received a placebo. Beano was significantly superior to the placebo in reducing flatus (gas in the stomach).
There was no difference between the two groups in terms of abdominal pain and bloating.27
Do digestive enzymes help relieve IBS symptoms?
Should you take digestive enzyme supplements or not? Well, digestive enzyme supplements are a good source for improving IBS and IBD symptoms, they seem to do too little to have any long-term beneficial effects.
Other supplements options to consider
Below is a summary of some of the other supplement options and relevant clinical information:
| Supplement | Quality of Information/Level of Confidence | Possible Mechanisms of Actions | Relevant Clinical Trials |
|---|---|---|---|
| Peppermint Oil | High for abdominal pain | Mainly antispasmodic | In as many as nine RCTs, the use of peppermint oil has proven to be superior to placebo in relieving abdominal pain in IBS and IBD.5152 |
| Slippery Elm | Low for IBD and IBS | Mainly antioxidant | There have been no human trials. The only available studies are in vitro (conducted in a lab on cells and tissues), where slippery elm has shown to have some antioxidant benefits.4950 |
| Green Tea (Polyphenols) | Low for IBD and IBS | Antioxidant, anti-inflammatory, barrier protection, microbiota improvement | A meta-analysis has shown a negative correlation between drinking green/herbal tea and IBD. However, the value of drinking green tea for relieving IBD or IBS symptoms or disease processes is unknown.48 |
| Magnesium | High for reducing gut inflammation | Mainly anti-inflammatory | Magnesium deficiency is a recognized complication of IBD. Moreover, the deficiency of magnesium seems to trigger disease progression itself by promoting gut inflammation. Magnesium supplementation, therefore, is strongly recommended in individuals with IBD.47 |
| Ginger | Low for IBD and IBS | Antioxidant, anti-inflammatory, immune boosting properties, and promotes microbiota | In one animal research, ginger extract supplement did produce encouraging results in terms of improving IBD symptoms and even reversed the disease pathology. However, there has been no relevant research conducted on humans.45 In IBS, however, ginger did not prove to be superior to placebo in providing symptomatic relief.46 |
| Boswellia | Low for IBD and IBS | Antioxidant and anti-inflammatory | Boswellia extract was found to be superior compared to sulfasalazine in an RCT conducted in 1997. However, in an RCT conducted in 2011, Boswellia was not found to be superior even to placebo in improving IBD symptoms or disease progression.4243. For IBS, Boswellia seems to provide symptomatic relief but has failed to demonstrate tremendous benefits.44 |
| Aloe Vera | High for IBD and IBS | Antioxidant, anti-inflammatory, protects the gut barrier, promotes the growth of microbiota | In one RCT, the effects of aloe vera were tested against placebo in patients with active ulcerative colitis. The aloe vera group was given 100 ml of aloe vera twice daily for 4 weeks. A significantly higher proportion of the participants in the aloe vera group achieved clinical and histological remission compared to the placebo.40 A meta-analysis has shown a significant improvement in the IBS symptoms and quality of life of IBS sufferers compared to placebo therapies.41 |
| Vitamin D | Medium for IBD and IBS | Anti-inflammatory | More than 64 % of individuals with IBD are deficient in Vitamin D.36 In RCTs, IBD sufferers when given Vitamin D supplements showed a reduction in the markers of inflammation. This might indicate a possible benefit of Vitamin D supplementation for IBD.37 In IBS, Vitamin D deficiency is a recognized feature. The data available to support the use of Vitamin D is mixed. Some studies have shown a significant improvement of IBS symptoms and quality of life and other studies have shown only a minor improvement in IBS symptoms with Vitamin D supplementation.3839 |
Supplements, IBS, and IBD: What works?
Being a gastroenterologist, I always encourage patients to focus on a healthy and well-balanced lifestyle first. IBS and IBD are complicated conditions – and there are a lot of things about these conditions that we still don’t understand.
Whenever my patients ask if they should try a certain supplement, I always encourage them to carry out their own research. The more you read, the more likely you are to know about your condition and the less likely you are to fall for pseudoscience.
Best supplements for IBS and IBD
The supplements that I have found to be effective for IBS and IBD in my own practice and based on my experience and research are: probiotics, Vitamin D, and magnesium.
The amount of research and data to support the use of fish oil, cbd oil, slippery elm, digestive enzymes, ginger, green tea, turmeric, aloe vera, and boswellia is insufficient.
- Ott SJ, Musfeldt M, Wenderoth DF, Hampe J, Brant O, Fölsch UR, Timmis KN, Schreiber S. Reduction in diversity of the colonic mucosa associated bacterial microflora in patients with active inflammatory bowel disease. Gut. 2004;53:685–693
- Johansson ME, Phillipson M, Petersson J, Velcich A, Holm L, Hansson GC. The inner of the two Muc2 mucin-dependent mucus layers in colon is devoid of bacteria. Proc Natl Acad Sci USA. 2008;105:15064–15069
- Martinez-Medina, M, Aldeguer X, Gonzalez-Huix F, Acero D, Garcia-Gil LJ. Abnormal microbiota composition in the ileocolonic mucosa of Crohn’s disease patients as revealed by polymerase chain reaction-denaturing gradient gel electrophoresis. Inflamm Bowel Dis. 2006;12:1136–1145
- Frank DN, St Amand AL, Feldman RA, Boedeker EC, Harpaz N, Pace NR. Molecular-phylogenetic characterization of microbial community imbalances in human inflammatory bowel diseases. Proc Natl Acad Sci USA. 2007;104:13780–13785
- Spiege lBM. Questioning the bacterial overgrowth hypothesis of irritable bowel syndrome: an epidemiologic and evolutionary perspective. Clin Gastroenterol Hepatol. 2011;9:461–49; quiz e59
- Jan Bures, et al. Small intestinal bacterial overgrowth syndrome. World J Gastroenterol. 2010 Jun 28; 16(24):2978–2990
- Niess JH. Role of mucosal dendritic cells in inflammatory bowel disease. World J Gastroenterol. 2008;14:5138–5148
- Baumgart DC, Carding SR. Inflammatory bowel disease: cause and immunobiology. Lancet. 2007;369:1627–1640
- Hart AL, Al-Hassi HO, Rigby RJ, Bell SJ, Emmanuel AV, Knight SC, et al. Characteristics of intestinal dendritic cells in inflammatory bowel diseases. Gastroenterology. 2005;129:50–65
- Cario E, Podolsky DK. Differential alteration in intestinal epithelial cell expression of toll-like receptor 3 (TLR3) and TLR4 in inflammatory bowel disease. Infect Immun. 2000;68:7010–701715
- Maeda S, Hsu LC, Liu H, Bankston LA, Iimura M, Kagnoff MF, et al. Nod2 mutation in Crohn’s disease potentiates NFkappaB activity and IL-1 beta processing. Science. 2005;307:734–73816
- Emanuele Sinagra, et al. Inflammation in irritable bowel syndrome: Myth or new treatment target? World J Gastroenterol. 2016 Feb 21; 22(7): 2242–2255
- Vecchi Brumatti L, Marcuzzi A, Tricarico PM, Zanin V, Girardelli M, Bianco AM. Curcumin and inflammatory bowel disease: potential and limits of innovative treatments. Molecules. 2014;19:21127–21153
- Kumar S, et al. Curcumin for maintenance of remission in ulcerative colitis. Cochrane Database Syst Rev. 2012 Oct 17;10:CD008424. doi: 10.1002/14651858.CD008424.pub2.
- Lang A, et al. Curcumin in Combination With Mesalamine Induces Remission in Patients With Mild-to-Moderate Ulcerative Colitis in a Randomized Controlled Trial. Clin Gastroenterol Hepatol. 2015 Aug;13(8):1444-9.e1. doi: 10.1016/j.cgh.2015.02.019. Epub 2015 Feb 24
- Sandra Maria Barbalho, et al. Inflammatory bowel disease: can omega-3 fatty acids really help? Ann Gastroenterol. 2016 Jan-Mar; 29(1): 37–43.23
- Yakoob, et al. Role of Omega-3 Fatty Acids in Irritable Bowel Syndrome (IBS). IJPR Volume 6 Issue 08 (2016)
- Turner D, et al. Maintenance of remission in inflammatory bowel disease using omega-3 fatty acids (fish oil): a systematic review and meta-analyses. Inflamm Bowel Dis. 2011 Jan;17(1):336-45. doi: 10.1002/ibd.21374
- Cabré E, et al. Omega-3 fatty acids and inflammatory bowel diseases – a systematic review. Br J Nutr. 2012 Jun;107 Suppl 2:S240-52. doi: 10.1017/S0007114512001626
- Arkadiusz Michalak, et al. Polyunsaturated Fatty Acids and Their Derivatives: Therapeutic Value for Inflammatory, Functional Gastrointestinal Disorders, and Colorectal Cancer. Front Pharmacol. 2016; 7: 459
- Waseem Ahmed, et al. Therapeutic Use of Cannabis in Inflammatory Bowel Disease. Gastroenterol Hepatol (N Y). 2016 Nov; 12(11): 668–679.
- Waseem Ahmed, et al. Therapeutic Use of Cannabis in Inflammatory Bowel Disease.Gastroenterol Hepatol (N Y). 2016 Nov; 12(11): 668–679
- Naftali T, et al. Cannabis induces a clinical response in patients with Crohn’s disease: a prospective placebo-controlled study. Clin Gastroenterol Hepatol. 2013 Oct;11(10):1276-1280.e1. doi: 10.1016/j.cgh.2013.04.034. Epub 2013 May 4
- Filippo Antonini, et al. Pancreatic disorders in inflammatory bowel disease. World J Gastrointest Pathophysiol. 2016 Aug 15; 7(3): 276–282
- Mary E Money, et al. Pilot study: a randomised, double blind, placebo controlled trial of pancrelipase for the treatment of postprandial irritable bowel syndrome-diarrhoea. Pilot study: a randomised, double blind, placebo controlled trial of pancrelipase for the treatment of postprandial irritable bowel syndrome-diarrhoea
- R. SPAGNUOLO1, et al. Beta-glucan, inositol and digestive enzymes improve quality of life of patients with inflammatory bowel disease and irritable bowel syndrome. European Review for Medical and Pharmacological Sciences 2017; 21 (2 Suppl): 102-107
- Ganiats TG, et al. Does Beano prevent gas? A double-blind crossover study of oral alpha-galactosidase to treat dietary oligosaccharide intolerance. J Fam Pract. 1994 Nov;39(5):441-5
Alcohol and its Effects on IBD and IBS
If you’re suffering from irritable bowel syndrome or an inflammatory bowel disease, you might wonder if drinking alcohol is going to make your symptoms worse. You’ve probably heard that alcohol is bad for your gut, but not sure to what extent. Depending on your specific condition, we have reviewed the effects of alcohol revealed by recent scientific research.
The Complete Guide to Ulcerative Colitis
Ulcerative colitis (UC) is one of two types of inflammatory bowel disease (IBD). UC, as its name implies, means ‘ulcers’ from inflammation of the colon or large intestine. UC can extend from the rectum up to the small intestine and can cause destruction of other organs.
Human Growth Hormone (HGH) Therapy for IBD
Introduction to Human Growth Hormone Human Growth Hormone (HGH) is mostly known for the dubious claim that it can slow aging, as well as its use by bodybuilders to accelerate muscle growth. HGH is an important hormone that stimulates and regulates our body’s growth and cell reproduction. Some people have HGH deficiencies, leading to stunted […]
Small Intestinal Bacterial Overgrowth (SIBO)
SIBO is a condition that brings about excess bacterial growth in the small bowel. Though there are many studies that have highlighted the efficacy of various treatments, more research needs to be done on other factors and alternative treatments that can prevent SIBO.
Symptoms of Crohn’s Disease in Females
Symptoms of Crohn’s disease in women are similar to men except that women are more prone to gynecologic disturbances in severe cases and may experience pregnancy difficulties if the symptoms are severe and the condition uncontrolled. Prompt diagnosis and treatment are essential for women throughout their reproductive years.
Irritable Bowel Syndrome (IBS) Symptoms in Women Aggravated by Hormones
Women have unique challenges to manage their IBS successfully. Symptoms of IBS in women vary wildly and underlying hormonal disturbances play a key role. There are multiple triggers that increase a woman’s susceptibility to flares of IBS.
The Specific Carbohydrate Diet (SCD Diet) for IBS and IBD
The Specific Carbohydrate Diet, or SCD Diet, is one of the longest researched lifestyle changes to alleviate life-threatening digestive issues. Beginning with the “Banana Diet,” developed nearly 100 years ago for children with celiac disease, the SCD diet quickly showed results for IBS and IBD.
Interview With Kristina Campbell, MSc, On The Gut Biome
An interview with gut biome expert, science writer Kristina Campbell (M.Sc.), the author of The Well-Fed Microbiome Cookbook and co-author of an academic textbook, Gut Microbiota: Interactive Effects on Nutrition and Health. She writes, consults, and works with scientific advisory boards for microbiome-related organizations throughout Europe and North America.
Cannabis to Treat Ulcerative Colitis and Crohn’s Disease
As many of us have realized, traditional treatments of ulcerative colitis, pancolitis, and Crohn’s disease are not effective for many patients. If you are not responding to traditional treatment or feel the medications you’re taking are doing more harm than good, you may want to consider using cannabis to treat your ulcerative colitis, pancolitis, or Crohn’s disease. Science has not yet demonstrated that cannabis is a cure. However, anecdotal evidence, the sheer number of patients with IBDs using marijuana, coupled with its low risk (besides legal in jurisdictions where it’s prohibited) and cost suggest that it’s worth trying if you haven’t responded to other treatments.
All about Gluten-Free Alcohol
If you’re suffering from irritable bowel syndrome or disease, you might wonder if there’s some miraculous way to get away with drinking alcohol. You likely already know to avoid alcohol as it may provoke an attack, but want to find a loophole. Depending on the specific condition, there may be certain types of alcohol that are safe, or at least safer.
The Carnivore Diet for Inflammatory Bowel Disease (IBD)
The Carnivore Diet is a member of the low-carb, high-fat (LCHF) diet family. Although not universally adopted by the science or medical community, and with a potentially complicated transition, it has had nearly universally positive results for those with Crohn’s, UC, and IBS dedicated enough to try it.
Fecal Microbiota Transplant (FMT) for Inflammatory Bowel Disease (IBD)
Fecal Microbiota Transplant (FMT) is a completely natural and safe process that, while a little weird, has led to remission of Crohn’s, Ulcerative Colitis, and IBS for many people. This is an introductory summary of what to expect, what you will need, and whether it’s for you.
Hyperbaric Oxygen Treatment (HBOT) for Inflammatory Bowel Disease (IBD)
Hyperbaric Oxygen Treatment is a technique famously used to heal decompression sickness or “the bends.” In the last decade it emerged as a safe treatment with success treating Crohn’s, Ulcerative Colitis, and IBS for many individuals.

Comments
One response to “Supplements for IBS and IBD: Is There Any Evidence?”
D
Thank you for this. Has your opinion changed in the last 2 years? What would you suggest for a 13 year old?